Physical Exam Template Soap Note
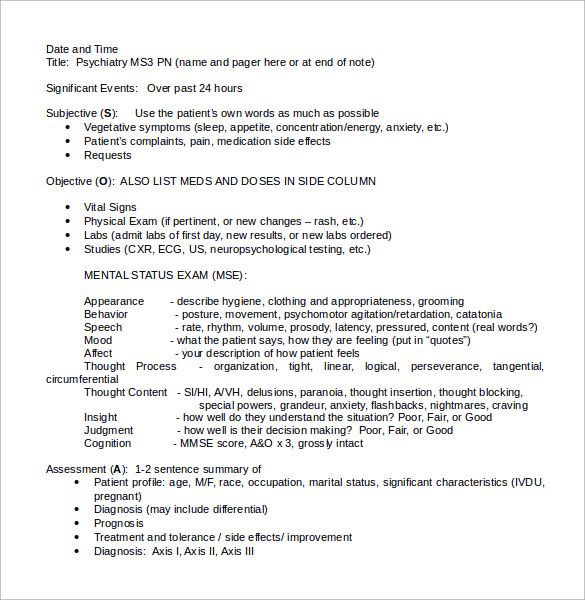
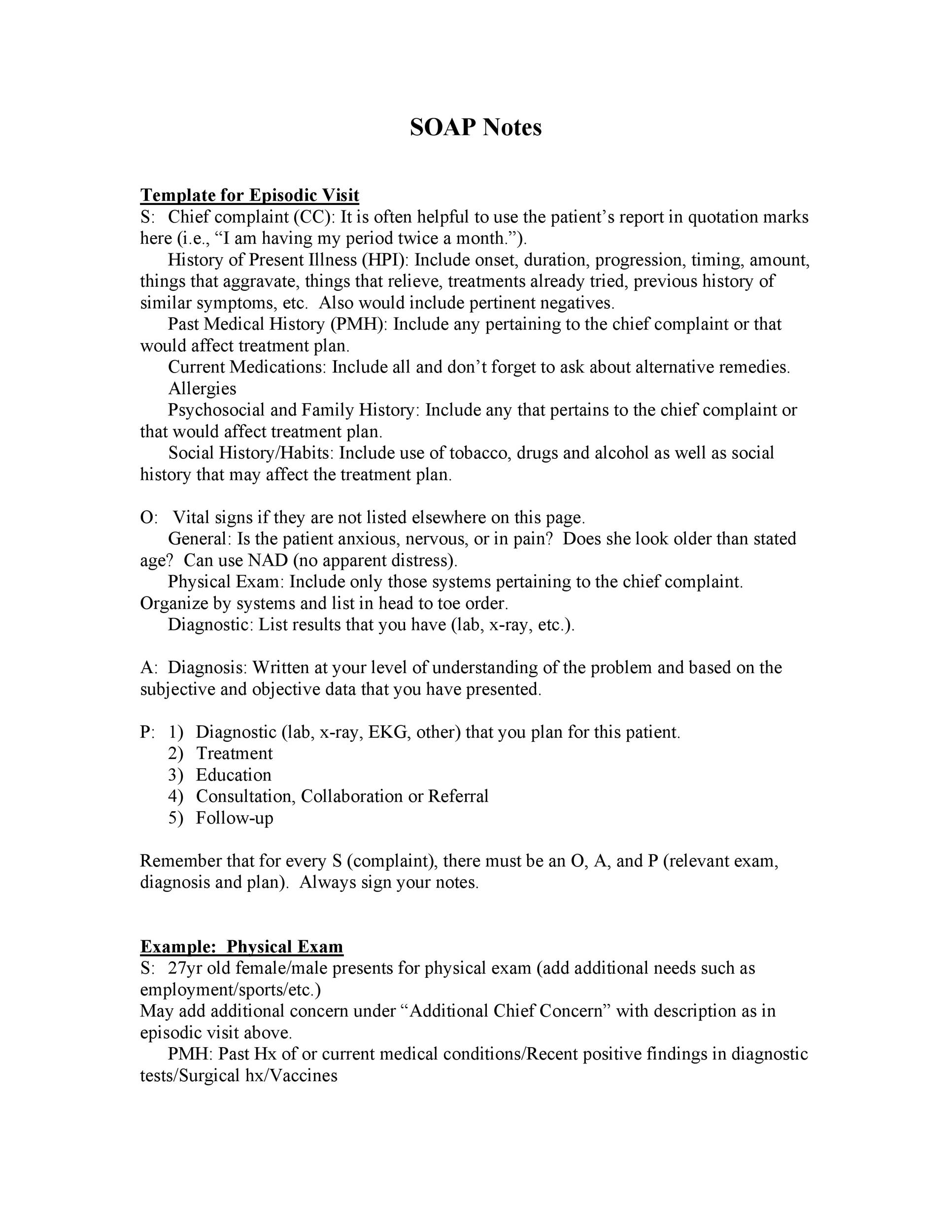
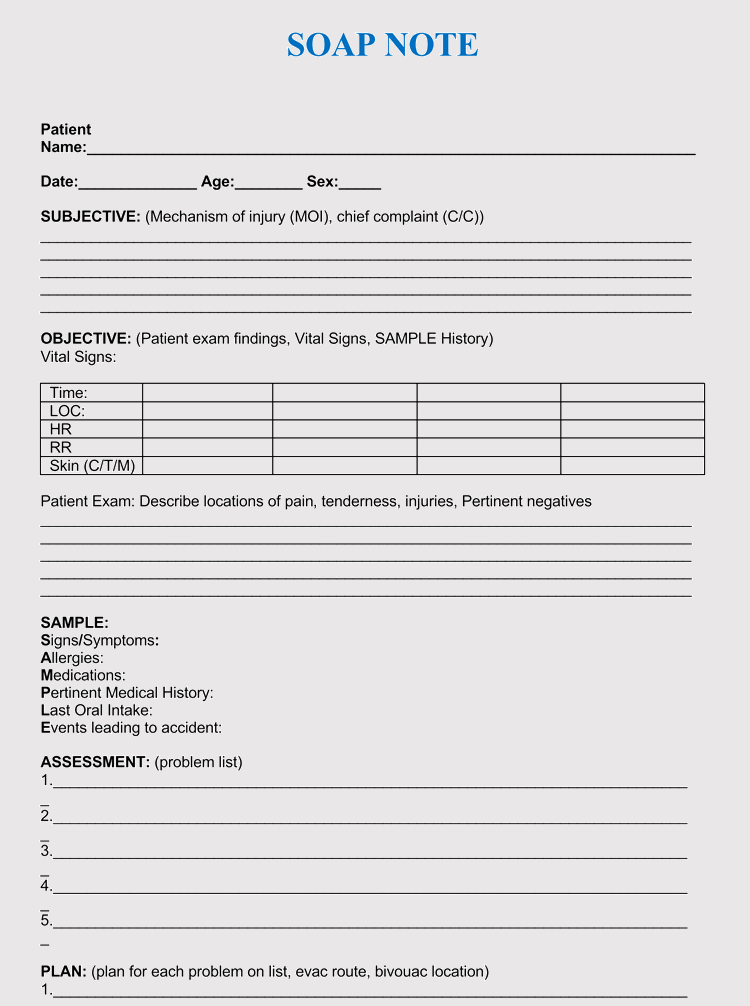
Physical Exam Template Soap Note - Web (listed are the components of the all normal physical exam) a: This is a pleasant, cooperative,. Author information and affiliations last update: Web soap notes vivek podder; Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for.
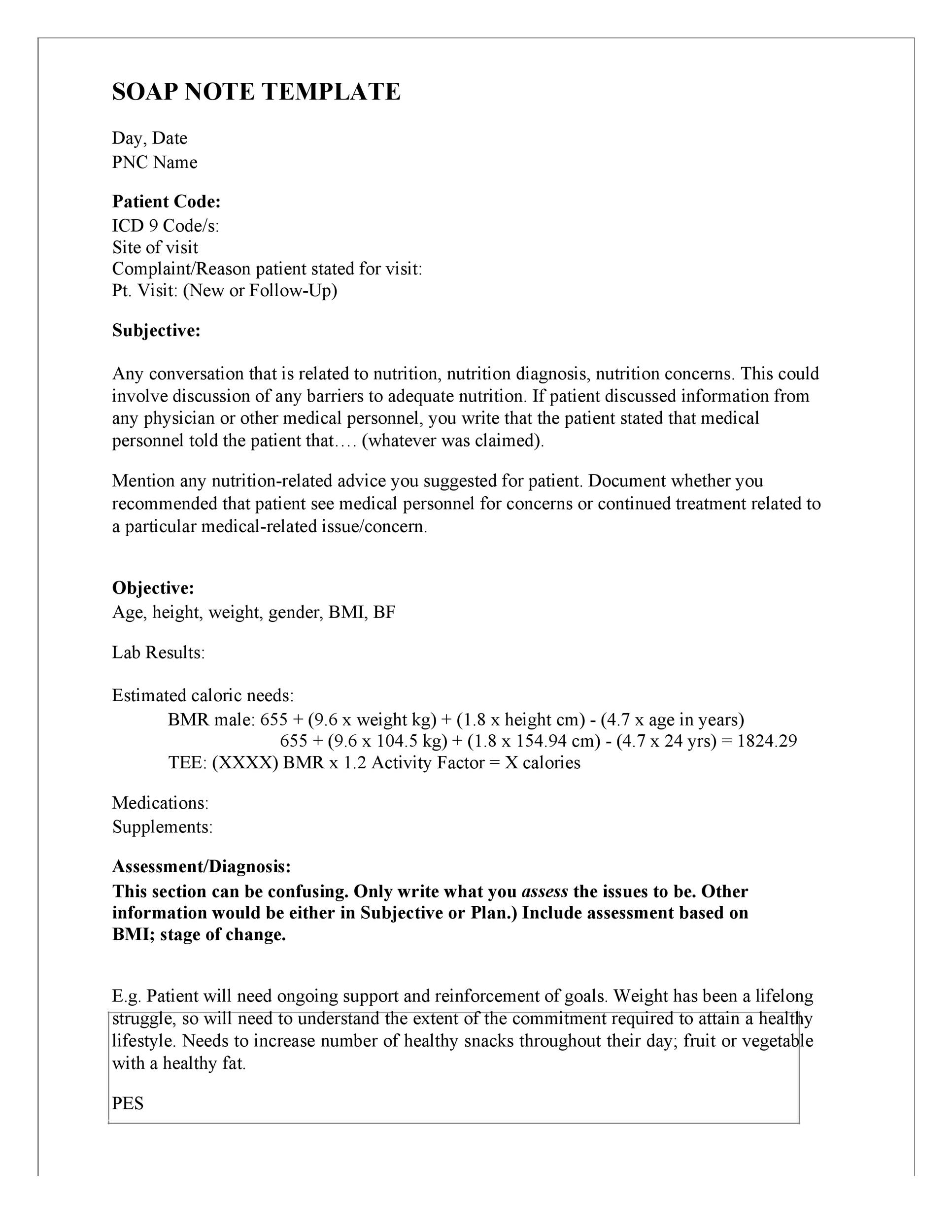
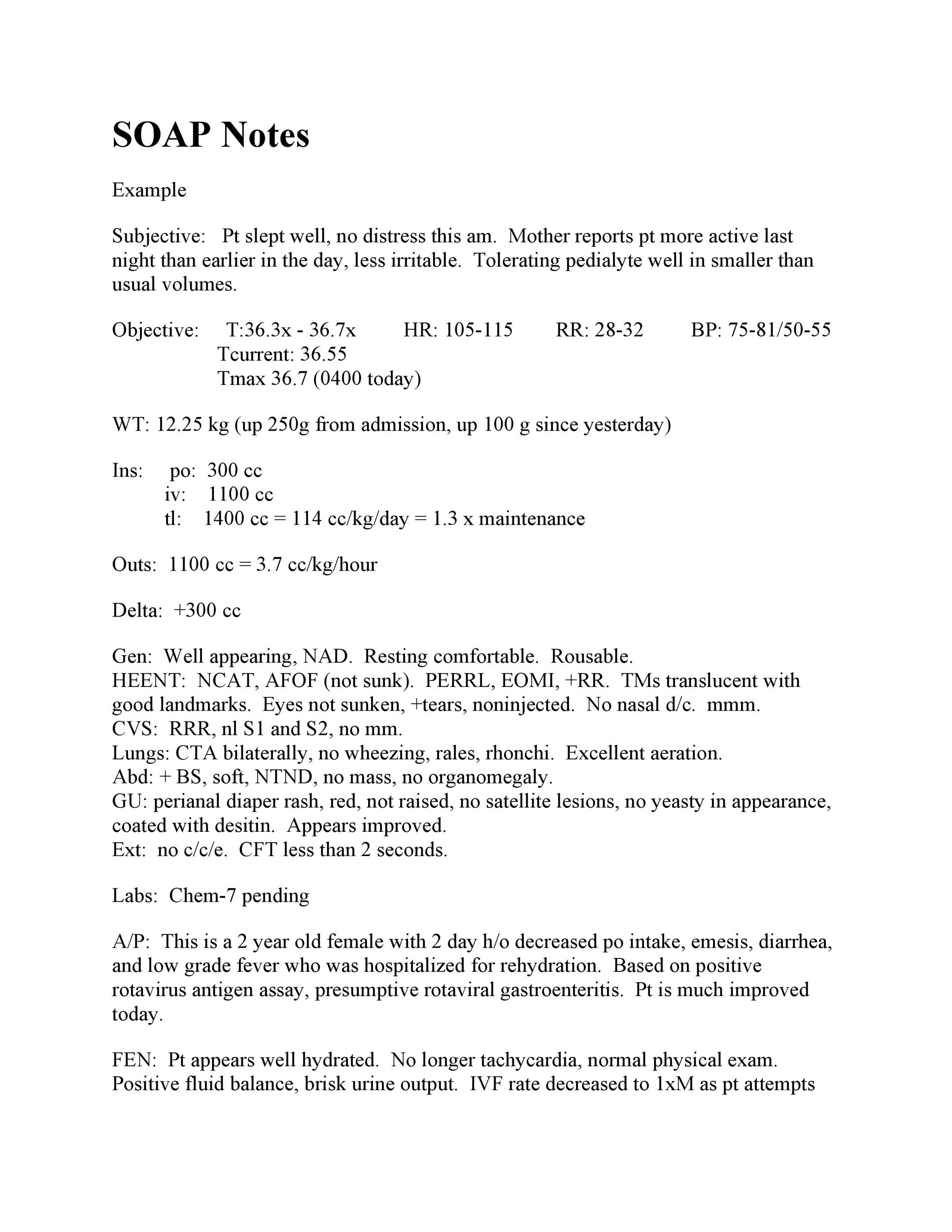
Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Approximately 560 views in the last month. This is a pleasant, cooperative,. Web nurses can use this soap note template to collect patient’s information for admission purposes. Here are the soap note templates that you. Alert and oriented x 3. Web “how are you today?” “how have you been since the last time i reviewed you?” “have you currently got any troublesome symptoms?” “how is your nausea?” if.
klauuuudia Pediatric Physical Exam Template
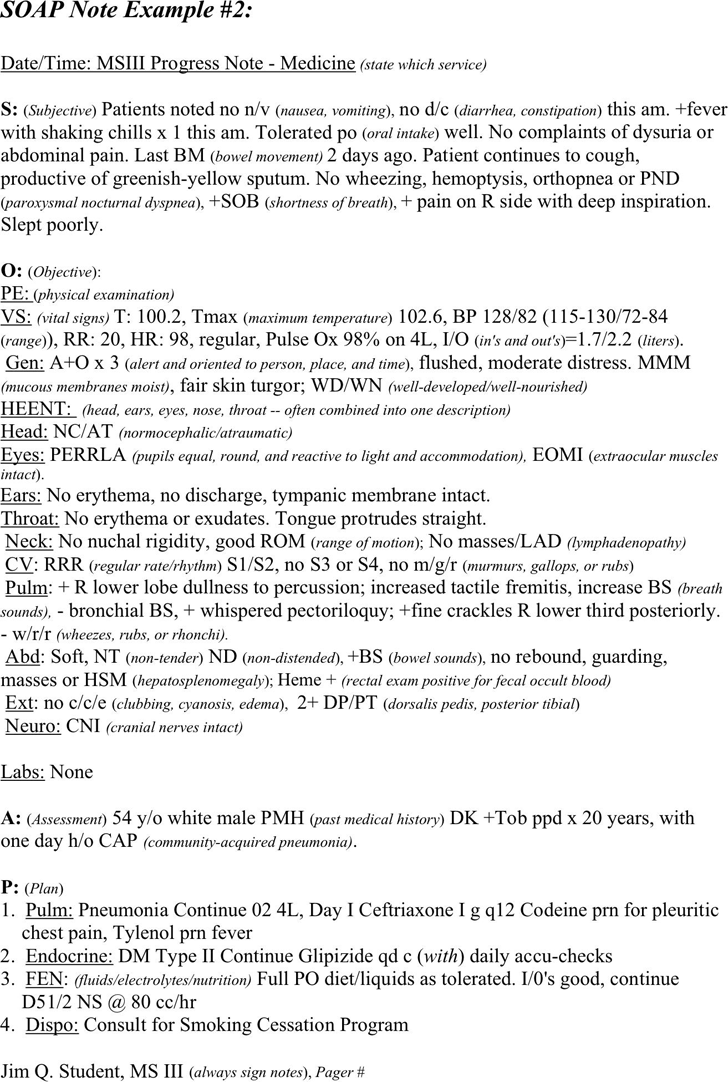
Web physical therapy soap note example (sample) to help you visualize what a completed soap note will look like using. Web nurses can use this soap note template to collect patient’s information for admission purposes. Web template for physical therapy soap notes here is a template you can use to guide your soap notes: Normal.
Free SOAP Note Example PDF 102KB 1 Page(s)
Web general adult physical exams. It’s meant to be a practical tool. This is a pleasant, cooperative,. The soap note template is a documentation method used by medical practitioners to assess a patient's. Web nurses can use this soap note template to collect patient’s information for admission purposes. Web finally (disclaimer alert!), this post is.
Physical Therapist SOAP Notes Example Soap note, Physical therapy
Web “how are you today?” “how have you been since the last time i reviewed you?” “have you currently got any troublesome symptoms?” “how is your nausea?” if. Web finally (disclaimer alert!), this post is not an exhaustive documentation reference. Web health professionals must have an accurate record of their patients. Web soap notes vivek.
Physical Therapy Soap Note For Stroke Patient United Health Care
Web general adult physical exams. Alert and oriented x 3. Web soap notes vivek podder; Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Normal physical exam template |. The soap note template is a documentation method used by medical practitioners to assess a patient's..
klauuuudia Pediatric Physical Exam Template
Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. This is a pleasant, cooperative,. Normal physical exam template |. Web the subjective,.
Comprehensive Physical Exam Template Sample Templates
Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Approximately 560 views in the last month. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of. Web template for physical therapy soap notes here is a.
How to Make Soap Notes Soap note, Soap making, Solution focused therapy
Web (listed are the components of the all normal physical exam) a: Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for. Approximately 560 views in the last month. Web this veterinary physical exam template is based on the soap template for a veterinary physical.
Physical Exam Soap Note Example
Web “how are you today?” “how have you been since the last time i reviewed you?” “have you currently got any troublesome symptoms?” “how is your nausea?” if. Web template for physical therapy soap notes here is a template you can use to guide your soap notes: Web physical therapy soap note example (sample) to.
Soap Report Template (8) TEMPLATES EXAMPLE TEMPLATES EXAMPLE Soap
Web physical exam normal medical template transcription samples. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Gastroenterology & hepatology, objective/exam elements. It’s meant to be a practical tool. Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used.
SOAP Note PDF Medicine Diseases And Disorders
Approximately 560 views in the last month. Web health professionals must have an accurate record of their patients. The soap note template is a documentation method used by medical practitioners to assess a patient's. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one.
Physical Exam Template Soap Note Web (listed are the components of the all normal physical exam) a: Web template for physical therapy soap notes here is a template you can use to guide your soap notes: Web general adult physical exams. Here are the soap note templates that you. Web health professionals must have an accurate record of their patients.
Web Template For Physical Therapy Soap Notes Here Is A Template You Can Use To Guide Your Soap Notes:
Web physical therapy soap note example (sample) to help you visualize what a completed soap note will look like using. Author information and affiliations last update: Alert and oriented x 3. This is a pleasant, cooperative,.
Web The Subjective, Objective, Assessment And Plan (Soap) Note Is An Initials Representing A Widely Used Method Of Documentation For.
Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Web physical exam normal medical template transcription samples. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Here are the soap note templates that you.
Web A Soap Note Is An Acronym Of Subjective, Objective, Assessment And Plan Which Represents A Method Of.
The soap note template is a documentation method used by medical practitioners to assess a patient's. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Web soap notes vivek podder; Web (listed are the components of the all normal physical exam) a:
It’s Meant To Be A Practical Tool.
Web nurses can use this soap note template to collect patient’s information for admission purposes. Web general adult physical exams. Approximately 560 views in the last month. Web “how are you today?” “how have you been since the last time i reviewed you?” “have you currently got any troublesome symptoms?” “how is your nausea?” if.